How PAS Affects Nurses
The author’s main purpose for this paper is to explain how physician assisted suicide (PAS) affects palliative care nurses providing care for quadriplegic patients. The author explains that because of learning barrier’s nurses often do not know how to approach this delicate topic.
Learning barriers include personal beliefs against physician assisted suicide, suicide terminology stigma, and lack of support from major nursing organizations. All nurses come from different backgrounds as explained, but all nurses must be aware of what PAS is and how to educate the patient on the laws surrounding PAS. The author also includes what behaviors can be assessed within patients at risk for depression and suicidal ideation, and how the patient’s chronic disability has affected the patient’s quality of life. Finally, the author elaborates on the nurse’s role in PAS in states that it is illegal and legal.
Physician Assisted Suicide Controversy
A major ethical topic, controversial in different regions of the world, is physician assisted suicide. Many argue that all life is important and valuable regardless of the cost or personal feelings. Others argue that it is a decision that should be kept between the patient and the primary physician. Regardless of society’s opinion, many important questions regarding the patient’s rights, nursing approach, and scope of health care practitioners are left up for debate. One of the biggest concerns being faced every day is the impact that physician assisted suicide (PAS) has on nursing and how to approach the delicate topic.
Palliative care nurses originate from wide demographic backgrounds with various cultural and religious beliefs, ethnic backgrounds, socioeconomic status, and various experience levels. Nurses providing palliative care come from different educational levels. The LPN level is obtained by a 2-year associate degree in nursing or a one-year diploma. The RN level is obtained by a 2-year associates degree in nursing or a 4-year Bachelor of Science in nursing degree. Palliative care nurses take specialized care courses to become certified in palliative care nursing (What is a Palliative Care Nurse?, 2019). Learning barriers for palliative care nurses include personal beliefs against physician assisted suicide, suicide terminology stigma, and lack of support from major nursing organizations (Barriers to Acceptance of Assisted Suicide, 2011). Methodology for presenting information to palliative care nurses will be presented through power-point presentation, open discussion, and an educational quiz to evaluate if learning has occurred.
Death with Dignity Acts
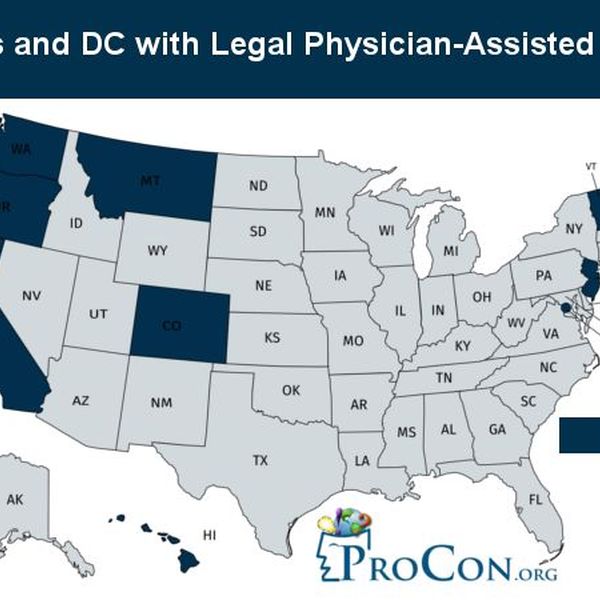
Physician assisted suicide (PAS) is a comfort care option available to end the life of someone suffering unbearable pain that causes the loss of quality of life. According to Nursing Today, several states have passed Death with Dignity acts to legalize physician assisted suicide including California, Colorado, Hawaii, Oregon, Washington, Vermont, and the District of Columbia (Zerwekh & Zerwekh Garneau, 2015). Each state has specific criteria that must be met for eligibility. According to How Death with Dignity Laws Work, the patient must be a resident of the state, be at least 18 years old, mentally competent, and diagnosed with a terminal illness that will cause death within six months. The patient must be able to administer life ending medication to themselves and two physicians must evaluate the patient. Evaluating the patient consists of the physician assessing the patient’s mental status, if the patient has depression, and if the patient can independently administer one’s medication. Also, the physician must make sure their diagnosis for death is within six months. If any of the eligibility requirements are not met, then the request will be denied without exception.
PAS Steps
Once residency has been established, the next step is to make a formal first oral request to the primary physician to use the death with dignity act medication to end life. The first request serves to allow two physicians to confirm that the patient meets the required criteria and is informed of all alternative treatments, palliative care options including hospice, pain medications available for comfort, and allows time to alert a relative of the choice to use the life ending medication. The patient is then required to make a second oral request, or written request in some states, to use the end of life medication. Once the second request has been made, the physician will provide a prescription for the medication to be filled at a pharmacy. The medication provided is a large dose of a barbiturate in most cases, which comes in powder form and must be administered directly by the patient and no one else. If patient loses the ability to swallow, they will no longer be eligible to use the medication (How Death with Dignity Laws Work, 2015). The first learning barrier associated with palliative care nurses regarding physician assisted suicide is personal beliefs of the nurse. Nurses may have personal beliefs that go against a patient’s decision to use physician assisted suicide. In this presentation, this learning barrier will be acknowledged by educating palliative care nurses on patients’ autonomy and quality of life issues surrounding the decision to use PAS (Zerwekh & Zerwekh Garneau, 2015).
Problems with Suicide
Suicide is a major problem in the United States and is the 10th leading causes of death (American Foundation for Suicide Prevention, 2019). According to the National Institute of Mental Health, people of all races, ages, genders, and ethnicities can be at risk for committing suicide (Suicide in America). Individuals at risk for suicidal ideation include those with depression, a substance abuse disorder, a history of physical or mental abuse, and someone with a terminal medical illness or chronic disability like quadriplegia. Behaviors that demonstrate suicidal ideation include expressing feelings of emptiness and hopelessness, anxiety and agitation, becoming withdrawn from family and friends, lack of appetite, change in sleeping habits, giving away personal possessions, and expressing thoughts and feelings regarding death (Suicide in America). The second learning barrier associated with palliative care nurses regarding physician assisted suicide is suicide terminology stigma. The term “suicide” causes negative public feelings and adds unnecessary stigma towards physician assisted suicide. These negative feelings could make people feel that they are against PAS because it is against their beliefs, whereas if PAS was called something like “physician aid-in-dying” or “death with dignity” people may view it differently. Currently, organizations are trying to change the terminology by phasing out the term “physician assisted suicide” to seek out different language that would be more acceptable to the public. “Aid-in-dying” is currently the phrase of choice for many assisted suicide activists (Barriers to Acceptance of Assisted Suicide, 2011).
Quality of Life
According to the Centers for Disease Control, quality of life is defined as a multidimensional concept that usually includes subjective evaluations of both positive and negative aspects of life and this definition encompasses domains such as health, employment, financial, educational, spirituality, physical, mental, and emotion (Health-Related Quality of Life, 2018). Quality of life is directly affected by a life debilitating prognosis like quadriplegia. There is a wide range of causes for quadriplegia such as car accidents, sports injuries, or cerebrovascular accidents and most commonly affect males 15 years of age to 35 (Loyola University Health System, 2017). Individuals who have quadriplegia have many physical changes that occur including; inability to move limbs below site of injury, heightened skin sensations, changes in bowel and bladder control, increased risk of infections like pneumonia, pressure ulcers, weight gain due to inactivity, emotional and relational stress, and breathing difficulty due to weakened muscles reducing chest expansion (Avery Biomedical Devices, 2019). The loss of independence and mobility and learning how to cope emotionally cause an altered quality of life for these patients. There are ways to help them attain the best quality of life possible such as learning new ways to cope through mediation or soothing music, building a support system of others that have a similar condition or a support group for quadriplegia, continuing to engage in hobbies and interests, and continuing to engage in relationships with friends and family (Christopher Reeve Foundation, 2019). When speaking of quality of life, it is important to understand that the health of caregivers play a direct role in the health and quality of life in patients. In a study analyzing the quality of life in spinal cord injuries some caregivers reported a higher stress and depression level than the patient (Lude, Kennedy, and Ballert, 2014). Having a strong support system is important in the overall health of a patient.
Nurse’s Role in PAS
The nurse’s role in PAS is a controversial topic currently being debated. The nurse should first examine his/her own personal values and beliefs as it relates to this topic. Afterwards, the nurse should assess each individual patient for depression and suicidal ideation. If a patient is depressed or suicidal, the nurse still has a duty to report and seek the proper assistance for the patient. The nurse should educate the patient about the laws of PAS in the state of North Carolina. A nurse in North Carolina would educate the patient that the law does not support PAS and provide options to patients on other comfort measures available that assist in reducing pain and suffering such as palliative care. In states where PAS is legal, the nurse should be educated on legal options within his/her state to provide objective data to the patient and their family. Nurses in states where PAS is legal need to make sure all channels of communication are open. For instance, families and providers need to be empathetic about the patient’s choices and the right to end life prolonging care and patients should not feel judgement from family or providers about their health care choices. Educating the patient on the laws of PAS and the requirements the patient must meet to be considered for PAS is a necessity for nurses in states where PAS is legal. There are benefits and drawbacks for using PAS and patients should be educated on those things. Patients should be fully aware of what PAS is and the methods used to aide in dying. There are alternative resources available to assist patients which includes comfort care, caregiver support, and support groups. Assessing what the patient needs and what education to provide for the patient is the biggest role of a nurse no matter what state one is in.
Another barrier palliative care nurses may be faced with is lack of support from major medical associations. The American Nurses Association (ANA) prohibits the participation from nurses in PAS. They state it is contradictory to “The Right to Self-Determination” which states that “nurses may not act with the sole intent to end life”. (American Nurses Association, 2015). The American Academy of Hospice and Palliative Medicine remains neutral on the topic. The Hospice and Palliative Nurses Association also advises that nurses not participate in PAS (Hamric, A. B., Schwarz, J. K., Cohen, L., Mahon, M., 2018). Due to the lack of support from major medical associations, nurses are unclear about what their role is in care for patients seeking PAS. It is important for nurses to remember that even in areas where PAS is illegal, they still have a duty to advocate for the needs of their patients. If the nurse is practicing in a state where PAS is legal, the nurse should provide the proper education and resources to the patient in a judgement free manner.
Conclusion
In conclusion, physician assisted suicide is a highly debated topic especially in cases of patients with paralysis. Learning barriers including personal beliefs against physician assisted suicide, suicide terminology stigma, and lack of support from major nursing organizations are only a few reasons why health care providers, mainly nurses, often have a hard time approaching PAS. Currently, there are no states in the United States that allow patients with any form of paralysis to participate in PAS. Health care professionals must know one’s own feelings, values, laws within their state, and take into consideration the patients’ feelings and autonomy. Health care providers participating in helping patients end their life is extremely controversial, but in a health care environment when patient autonomy is highly valued should we reconsider? There are several countries around the world that are attempting to answer that question, and as healthcare providers we must be open to advocate for the needs of our patients.
References
- American Foundation for Suicide Prevention. (2019). Suicide Statistics. Retrieved from American Foundation for Suicide Prevention: http://afsp.org/about-suicide/suicide-statistics/
- Avery Biomedical Devices. (2019). What You Should Know About Quadriplegia. Retrieved from Avery Biomedical Devices: www.averybiomedical.com/what-you-should-know-quadriplegia/
- Barriers to Acceptance of Assisted Suicide. (2011). Retrieved from Life Resources Charitable Trust: http://www.life.org.nz/euthanasia/abouteuthanasia/abouteuthanasia1/Default.htm
- Christopher Reeve Foundation. (2019). Resources for Caregivers. Retrieved from Christopher & Dana Reeve Foundation: Christopherreeve.org/living-with-paralysis/for-caregivers/tips-and-resources-for-caregivers
- How Death with Dignity Laws Work. (2015). Retrieved February 15, 2019, from DeathwithDignity.org: http://www.Deathwithdignity.org/learn/access/
- Last Name, F. M. (Year). Article Title. Journal Title, Pages From – To.
- Last Name, F. M. (Year). Book Title. City Name: Publisher Name.
- Loyola University Health System. (2017, February 16). Spinal cord injury patients face many health problems besides paralysis. Retrieved from Science Daily: www.sciencedaily.com/releases/2017/02/170216103931.htm
- What is a Palliative Care Nurse? (2019). Retrieved February 18, 2019, from Registerednurses.org: https://www.registerednursing.org/specialty/palliative-care-nurse/
- Zerwekh, J., & Zerwekh Garneau, A. (2015). Nursing Today Transitions and Trends. St. Louis: Elsevier.